Baby Kaiba seemed healthy, but when he was six weeks old, his parents were shocked to the core. The family was dining at a restaurant, when the little boy suddenly stopped breathing, and his face turned blue due to lack of oxygen. In the hospital, doctors discovered that the cartilage of one of the boy’s bronchi – the two large windpipe branches – was unusually weak, so the walls of the pipe had collapsed and shut off his oxygen supply.
The boy’s doctor, Glenn Green from the US University of Michigan, had to place a tube through the bronchus, allowing air to be constantly blown directly into the lung. The solution was not a long-term one, but the doctor realized that he needed a specific spare part, which could keep the bronchus permanently open. Glenn Green had a vague idea of the make-up of the spare part, but he did not know where to get it. He looked at the printer in his office and came up with a good idea.
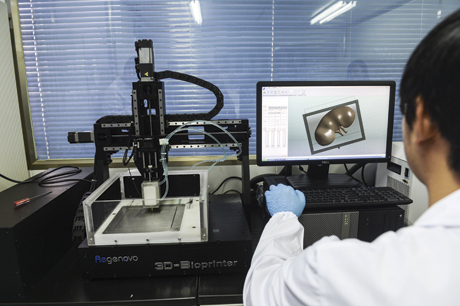
An ordinary ink jet printer is an ideal device, because it can print any combination of letters of any size or type – not to mention all types of images in all sorts of colours. But the 3D printer goes one step further, as it is able to copy almost any object by having the jets print plastic. The basic structure of the object is printed in layers, and it literally grows from the surface. Many spare parts or special gadgets can be difficult and expensive to make if they need to be cast, assembled, or cut out. But armed with a 3D printer, scientists only need to take a few photographs of the object from different angles, allow a computer to make a 3D model of it, and then hit the print button. Glenn Green immediately acted on the idea and used computer software to design the very spare part which could give Kaiba normal life once again.
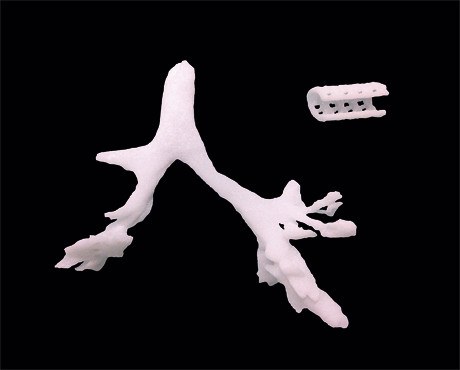
The solution consisted of a short tube with a slightly larger diameter than the bronchus and with a cut through it, allowing it to be opened and placed around the constricted part of the bronchus. The tube had to be perforated with small holes, making it easy to stitch to the weak wall of the bronchus, so it could be kept inflated. Once the design had been completed, the doctor poured biodegradable plastic into the 3D printer, and shortly afterwards he held the spare part in his hands – ready to be transplanted into baby Kaiba’s body.
The 3D printed spare part had the desired effect. Seven days after the surgery, doctors began to get the little boy used to breathing by himself. After three weeks, they were able to remove the air tube which had kept him alive by blowing air directly into his lungs. Ever since, the boy has been breathing nor-mally. As the spare part gradually degrades, the bronchus cartilage wall can regenerate, and after three years, it should be able to function independently.
Can save thousands of lives
Other doctors have taken this technology one step further, trying to upgrade the 3D printer so it will not only be able to produce “dead” spare parts, but also living copies tiusse which can carry out the original organ’s job. The aim is to make hospitals and patients independent of the long waiting lists for donor organs. In the EU and the US, 14,000 people die annually because they do not receive an organ in time. If 3D printing of organs really becomes a hit, many lives can be saved.
The organs can be printed in different ways, but there are two basic techniques. Either the scientists print a mould or they print the organ itself. In the case of the first option, the 3D printer prints a biodegradable material, producing a mould of the organ on which scientists place living cells. As the cells grow and ”settle down”, the mould degrades and finally only a living copy of the organ is left. The technique is best-suited for organs, which primarily consist of a single cell type, such as the nose or ears, whichare mainly made of cartilage cells.
However, some scientists have used the printer to print tube-shaped moulds with two sides, an internal and an external. They intend to place different cell types on the two sides, and later, when the mould has degraded the cells grow together. This makes it basically possible to produce intestines which consist of mucosa cells on the inside and muscle cells on the outside. But no scientists have achieved this yet.
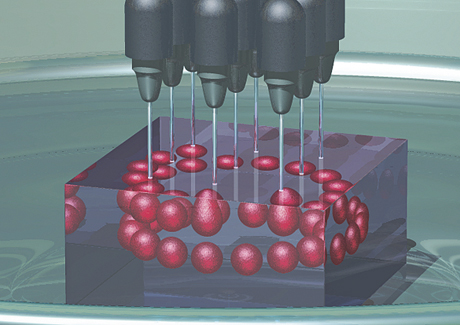
The other fundamental technique does not require a mould for the cells to grow on. Instead, the organ is printed directly by using living cells instead of ink. Just like an ordinary printer features several ink cartridges with different colours, the 3D printer can be equipped to use different cell types.
One of the cartridges often contains a sticky gel, which holds the cells together and fills up the cavities at for example the centre of blood vessels. The 3D printer deposits the gel and the different cell types in complex patterns and layers, and then the gel is dissolved. The 3D organ remains. The technique is quite promising, but still very much in development. So far, it has only been used to produce simple versions of organs such as skin and blood vessels.
The reputable chemist Leroy Cronin from the University of Glasgow in Scotland has other ambitions concerning the use of 3D printers. He expects the devices to revolutionise the way in which patients are treated in the near future. Back in 2012 he demonstrated how to print your own medication at home, so pharmacies could basically be rendered superflous.
Along with the prescription for a drug, the doctor could supply the patient with a computer file with the drug formula, which is based on simple chemicals. The file also contains the design of the device, which is needed to carry out the chemical reactions.
When the patient has hooked up his private 3D printer, he can hit the print button and watch a “miniature lab” be produced, complete with small containers for the necessary ingredients and channels, which bring the ingredients together and mix them, before they are directed to the reaction chamber.
During the next stage, the plastic of the printer cartridges is replaced by simple chemicals, and the printer doses the necessary ingredients at the right time and in the right places. In a few hours, the patient has printed the drug prescribed by the doctor without ever leaving his home (just like in the good old days!).
Leroy Cronin expects the technique to result in better treatment of people, who live in remote areas without a pharmacy nearby. The method will probably also lead to lower prices, as drug makers save money, which would otherwise have been spent on factories, packaging, distribution, and storage.
If Leroy Cronin’s expectations prove correct, we can soon begin to clear out our private medicine cupboards and make room for a 3D printer. The packet of adhesive plaster may also be thrown out one day, when we are able to close a wound by means of a patch of skin, printed using our own cells.